Ikke alt, som gør ondt, er en skade!
Af Morten Høgh, Ph.D. M.Sc.Pain, specialist i sportsfysioterapi | Adjunkt på Aalborg Universitet, Musculoskeletal Health and Implementation, Health Science and Technology, Medicinsk fakultet.
Kontakt: msh@hst.aau.dk / Twitter @mh_dk
Mange atleter oplever, at smerte forringer eller begrænser dem i deres sport. Og såvel atleter som professionelle kan have svært ved at adskille idræts-relaterede smerter fra idræts-relaterede skader. Traditionelt er smerte blevet opfattet som et udtryk for en skade, der kræver specifik behandling. I dag ved vi, at behandling af smerte og skade adskiller sig fra hinanden, og at smerte både kan og vil opstå uden skader i bevægeapparatet. Som professionel skal man derfor kunne forstå, forklare og håndtere såvel skader som smerte, herunder kunne vejlede atleten til at reagere forskelligt på smerter, der opstår sammen med hhv. uden en vævsskade.
Baggrund: Sammen med Michael Rathleff, Kristian Lyng og Sabina Vistrup undersøgte vi hvordan ”idrætsskade” (eng. sports injury) var anvendt i de randomiserede lodtrækningsforsøg, som var publiceret i BJSM fra oprindelsen til marts 2021. Vi fandt at smerte (pain) og skade (injury) bliver brugt i flæng, endda i samme manuskript (se appendix 1). Derfor satte vi os sammen med prof Steven Z George (US) og a/prof Tash Stanton og lavede vi en Infographic (produceret af Madeline Thorpe, AUS), der efterfølgende er blevet publiceret i BJSM (1). Denne artikel er en narrativ gennemgang af rationalet bag publikationen.
Baggrund (boks): Sammen med Michael Rathleff, Kristian Lyng og Sabina Vistrup undersøgte vi hvordan ”idrætsskade” (eng. sports injury) var anvendt i de randomiserede lodtrækningsforsøg, som var publiceret i BJSM fra oprindelsen til marts 2021. Vi fandt at smerte (pain) og skade (injury) bliver brugt i flæng, endda i samme manuskript (se appendix 1). Derfor satte vi os sammen med prof Steven Z George (US) og a/prof Tash Stanton og lavede vi en Infographic (produceret af Madeline Thorpe, AUS), der efterfølgende er blevet publiceret i BJSM (1). Denne artikel er en narrativ gennemgang af rationalet bag publikationen.
I denne artikel vil jeg argumentere for 1) at smerte ikke bør betragtes som en skade, 2) at smerte er en naturlig konsekvens af skade, 3) at smerte kan og vil opstå i fravær af skader, 4) at væv kan gå i stykker, men ikke gøre ondt og 5) at ovenstående er klinisk relevant.
Smerte og skade er ikke, og bør ikke anses som, synonymer
At skade ikke er afgørende for, at man oplever smerte har været kendt i mange år og indgår bl.a. i definitionen af smerte (2). Ikke desto mindre bruger mange forfattere smerte (pain) og skade (injury) synonymt, ligesom der er inkonsistens i, hvornår man burde bruge det ene eller andet til at afrapportere, hvorfor atleter ikke kan deltage i deres sport (se appendix 1). Vi foreslår, at man anvender begrebet sports-relateret skade, når undersøgelsen viser vævsskade, samt når der er en stærk, klinisk mistanke om en skade (fx tegn på inflammation, kendt skadesmekanisme eller visuelle fejlstillinger/forandringer).
Overordnet set er det den professionelle, der bedst kan vurdere, om atleten har fået en skade: I mange tilfælde kan den professionelle afgøre om der er tale om en skade på baggrund af en grundig klinisk undersøgelse, selvom parakliniske undersøgelser kan være nødvendige. Omvendt er smerte en oplevelse, som kun atleten kan redegøre for.
Figur 1: Sports-relateret skade vs sports-relateret smerte
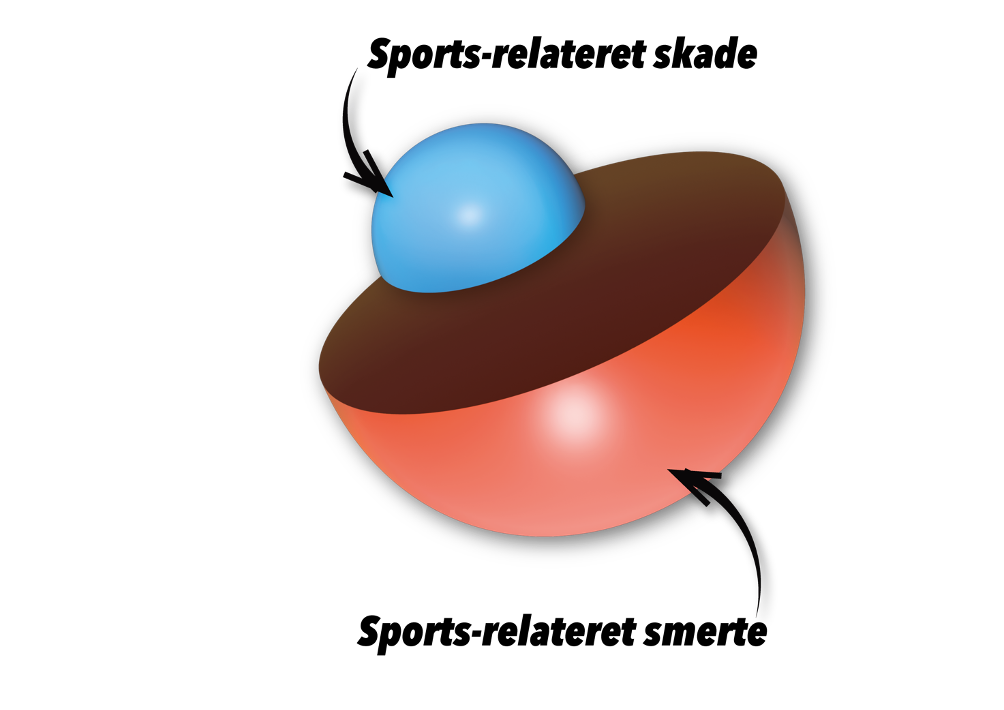
Figur 1 illustrerer at skader (blå) og smerte (rød) er forskellige og at skade i udgangspunktet altid vil medføre smerte, men at smerte kan eksistere helt uden skade. Størrelsesforholdet er fiktivt, men det formodes at forekomsten af sports-relaterede smerter er markant større end forekomsten af sports-relaterede smerter. En partiel ligament-ruptur (type II) er et eksempel på en skade, der også medfører smerte i den akutte fase hvor der er inflammation. Og patellofemorale smerter er et eksempel på en smerte, der ikke er relateret til en skade på vævet.
Som det fremgår af Figur 1 formodes smerte at kunne opstå uden skade, mens skade i udgangspunktet vil medføre smerte. Og derfor skal klinikeren være i stand til at vurdere, om vævsskaden er den bedste/eneste forklaring på atletens smerte, og derfor om smerten vil forventes at forsvinde helt når skaden er helet. Hvis vævsskade er den bedste forklaring på smerten, vil det være rationelt af fokusere på, og lade behandlingen være styret af, helingen, samtidig med at atleten kontrollerer smerten (som må forventes at være aftagende og sandsynligvis helt fraværende lang tid før en vævsskade er helet). Hvis atletens smerter ikke kan forventes at blive mindre i takt med forandringer i vævet, bør behandlingen primært fokusere på at smertelindre og på at støtte atleten i at få kontrol over smerterne, sideløbende med at denne vender tilbage til sport. Hermed ikke sagt, at vævsrettet behandling (fx træning) er irrelevant, men blot at øget styrke ikke kan forventes at lede til fuld og varig bedring (3,4).
Smerte er en naturlig konsekvens af skade
Inflammation er en fællesnævner for såvel sports-relateret skade og sports-relateret smerte, selvom sports-relateret smerte forekommer hyppigt uden inflammation og skade (5).
I forbindelse med skader er inflammationen en del helingen, men også afgørende for at vi får ondt (6): Dette illustreres bl.a. gennem relationen mellem prostaglandin og sensibilisering. Prostaglandin er et signalstof, der dannes gennem metaboliseringen af arakidonsyre via COX-1 og COX-2 (7). Prostaglandin E2 er særlig interessant fordi den påvirker nerveceller (”nociceptorer”) via EP2-receptoren, og som kan lede til ændringer af både receptorer og ion-kanaler (dvs. perifer sensibilisering). Sensibiliseringen anses for at være den primære grund til smerten, som patienten oplever i forbindelse med inflammation.
Væv kan gå i stykker uden at medføre smerte
Som det fremgår ovenfor, er det ikke vævsskaden, der i sig selv ”gør ondt”. Det er mere korrekt at sige, at smerten opstår som en konsekvens af reversible forandringer i nervesystemet. Det er med andre ord konsekvensen af skaden (især den inflammatoriske proces), der bedst forklarer, hvorfor en vævsskade medfører smerte. Det er således ikke blot semantisk uheldigt, men faktuelt forkert, at påstå at muskler, sener, led m.v. gør ondt. Vi anbefaler i stedet, at man beskriver strukturen (fx ACL), når man taler om skaden, og lokaliteten (knæet) når man taler om smerten. Dette tjener flere formål hvoraf de to væsentligste, i min optik, er at minde patienten om, at skaden og smerten er to forskellige ting, og at gøre det samme for klinikeren, så begge dele adresseres i relevant omfang.
Smerte kan og vil opstå i fravær af skader
Atleter har mindst lige så stor chance for at opleve uspecifikke smerter som baggrundsbefolkningen (8), og der er konsensus om, at denne type smerter ikke kan forklares blot som resultatet af én enkelt årsag, men derimod som resultatet af mange, gensidigt påvirkende faktorer (9). Ikke desto mindre er det biomekanik, der præger sportsmedicinens forklaringsmodeller (10), hvilket bevirker, at forekomsten af diagnoser af tvivlsom værdi er alt for høj (11). Det er imidlertid veldokumenteret at fx degeneration ikke er årsag til smerte (12–14), og at ensidigt fokus på at finde en ”smertegivende struktur” kan lede til overbehandling og måske have iatrogene konsekvenser i form af forlænget eller forringet tilbagevenden til idræt (15–18).
Inden for smerteforskningen forklares smerter uden kendt patogenese ofte som et resultat af forandringer i det centrale nervesystem (19). Disse såkaldte nociplastiske smerter (20) er udtryk for en ikke-veldefineret gruppe af mekanismer, inklusiv central sensibilisering, som ikke nødvendigvis er eksklusive for nociplastiske smerter, men som har det til fælles, at de ændrer på signaler fra kroppen således, at de fx ankommer med forstærket intensitet til hjernen, hvor de kan medføre øget smerteoplevelse. Nociplastiske smerter er derfor ikke en diagnose, men en teoretisk forklaringsmodel, der bl.a. skal gøre op med fejlslutninger som fx at smerterne har en psykisk årsag. Smerte er – i al sin kompleksitet – en oplevelse, som aldrig kan underkendes eller afvises, uanset om årsagen forekommer åbenlys eller ej (2). Når smerter opstår uden relevant skade, bør fokus i behandlingen rette sig mod at bevare atletens funktionsniveau (fx ved at undgå unødvendige pauser) og lære atleten at håndtere sine smerter med de midler, der har lavest risiko for bivirkninger og utilsigtede konsekvenser (21).
Hvad er nyt?
Smerte, som opstår ofte uden synlig/specifik skade, bør ikke behandles med de samme metoder, som man anvender til at behandle vævsskade. Derimod bør fokus rettes mod at fjerne eller lindre smerten, samt eliminere/reducere obstruktioner som smerten giver atleten. Et eksempel kan være tilpasset træningsplan ift at tillade atleten bedre søvn, hvis dette er en effektiv måde at tackle smerterne på, for den enkelte atlet. For den professionelle vil dette muligvis betyde ændringer i daglig praksis i det, fx i form af behov for at lære/rutinemæssigt anvende andre interventioner (fx uddannelse og vejledning i smertehåndtering) således at atleten bliver kompetent til at forstå og håndtere smerterne på egen hånd.
Vigtigste punkter for klinisk praksis:
En grundig klinisk undersøgelse med mulighed for parakliniske undersøgelser, når det er nødvendigt, er afgørende for at identificere specifik og/eller alvorlig patologi, som kræver specifik behandling. Men det tyder på, at flertallet af de muskuloskele problemer, som atleter henvender sig med, er smerte-relaterede. Smertelindring/-håndtering har mange facetter (fx hvile, varme, bevægelse eller distraktion) og behøver ikke omfatte regulering af atletens ”load”, selvom det ofte kan være et relevant.
Referencer
1. Hoegh M, Stanton T, George S, Lyng KD, Vistrup S, Rathleff MS. Infographic. Pain or injury? Why differentiation matters in exercise and sports medicine. Br J Sports Med. 16. september 2021;bjsports-2021-104633.
2. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, m.fl. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. september 2020;161(9):1976–82.
3. Messier SP, Mihalko SL, Beavers DP, Nicklas BJ, DeVita P, Carr JJ, m.fl. Effect of High-Intensity Strength Training on Knee Pain and Knee Joint Compressive Forces Among Adults With Knee Osteoarthritis: The START Randomized Clinical Trial. JAMA. 16. februar 2021;325(7):646.
4. Clausen MB, Hölmich P, Rathleff M, Bandholm T, Christensen KB, Zebis MK, m.fl. Effectiveness of Adding a Large Dose of Shoulder Strengthening to Current Nonoperative Care for Subacromial Impingement: A Pragmatic, Double-Blind Randomized Controlled Trial (SExSI Trial). Am J Sports Med. september 2021;49(11):3040–9.
5. Hainline B, Derman W, Vernec A, Budgett R, Deie M, Dvořák J, m.fl. International Olympic Committee consensus statement on pain management in elite athletes. Br J Sports Med. september 2017;51(17):1245–58.
6. Ji R-R, Xu Z-Z, Gao Y-J. Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov. juli 2014;13(7):533–48.
7. Wang B, Wu L, Chen J, Dong L, Chen C, Wen Z, m.fl. Metabolism pathways of arachidonic acids: mechanisms and potential therapeutic targets. Signal Transduct Target Ther. december 2021;6(1):94.
8. Fett D, Trompeter K, Platen P. Back pain in elite sports: A cross-sectional study on 1114 athletes. Smith B, redaktør. PLOS ONE. 29. juni 2017;12(6):e0180130.
9. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, m.fl. What low back pain is and why we need to pay attention. The Lancet. juni 2018;391(10137):2356–67.
10. Thornton JS, Caneiro JP, Hartvigsen J, Ardern CL, Vinther A, Wilkie K, m.fl. Treating low back pain in athletes: a systematic review with meta-analysis. Br J Sports Med. 21. december 2020;bjsports-2020-102723.
11. Friedman DJ, Tulloh L, Khan KM. Peeling off musculoskeletal labels: sticks and stones may break my bones, but diagnostic labels can hamstring me forever. Br J Sports Med. 6. maj 2021;bjsports-2021-103998.
12. Bezuglov E, Lazarev A, Petrov A, Brodskaia A, Lyubushkina A, Kubacheva K, m.fl. Asymptomatic Degenerative Changes in the Lumbar Spine Among Professional Soccer Players. Spine. 15. januar 2021;46(2):122–8.
13. Thompson SM, Fung S, Wood DG. The prevalence of proximal hamstring pathology on MRI in the asymptomatic population. Knee Surg Sports Traumatol Arthrosc. januar 2017;25(1):108–11.
14. Connolly M, Rotstein AH, Roebert J, Grabinski R, Malara F, O’Shea T, m.fl. Lumbar spine abnormalities and facet joint angles in asymptomatic elite junior tennis players. Sports Med – Open. december 2020;6(1):57.
15. Maher CG, O’Keeffe M, Buchbinder R, Harris IA. Musculoskeletal healthcare: Have we over‐egged the pudding? Int J Rheum Dis. november 2019;22(11):1957–60.
16. Salamh P, Lewis J. It Is Time to Put Special Tests for Rotator Cuff–Related Shoulder Pain out to Pasture. J Orthop Sports Phys Ther. maj 2020;50(5):222–5.
17. Shraim BA, Shraim MA, Ibrahim AR, Elgamal ME, Al-Omari B, Shraim M. The association between early MRI and length of disability in acute lower back pain: a systematic review and narrative synthesis. BMC Musculoskelet Disord. december 2021;22(1):983.
18. Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. Iatrogenic Consequences of Early Magnetic Resonance Imaging in Acute, Work-Related, Disabling Low Back Pain: Spine. oktober 2013;38(22):1939–46.
19. Shraim MA, Massé-Alarie H, Hodges PW. Methods to discriminate between mechanism-based categories of pain experienced in the musculoskeletal system: a systematic review. Pain. april 2021;162(4):1007–37.
20. Kosek E, Cohen M, Baron R, Gebhart GF, Mico J-A, Rice ASC, m.fl. Do we need a third mechanistic descriptor for chronic pain states? Pain. juli 2016;157(7):1382–6.
21. Cohen KR. Management of Chronic Low Back Pain. JAMA Intern Med [Internet]. 20. december 2021 [henvist 2. januar 2022]; Tilgængelig hos: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2787206
Appendix 1
| Reference | Pain | Injury | Mix of both |
| Paavola M, Kanto K, Ranstam J, et al. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: a 5-year follow-up of a randomised, placebo surgery controlled clinical trial. Br J Sports Med. 2021;55(2):99-107. | X | ||
| Roddy E, Ogollah RO, Oppong R, et al. Optimising outcomes of exercise and corticosteroid injection in patients with subacromial pain (Impingement) syndrome: a factorial randomised trial. Br J Sports Med. 2021;55(5):262-271. | X | ||
| Rasenberg N, Bierma-Zeinstra SMA, Fuit L, et al. Custom insoles versus sham and GP-led usual care in patients with plantar heel pain: results of the STAP-study – a randomised controlled trial. Br J Sports Med. 2021;55(5):272-278. | X | ||
| McGuine T, Post E, Pfaller AY, et al. Does soccer headgear reduce the incidence of sport-related concussion? A cluster, randomised controlled trial of adolescent athletes. Br J Sports Med. 2020;54(7):408-413. | X | ||
| Snoeker BA, Roemer FW, Turkiewicz A, Lohmander S, Frobell RB, Englund M. Does early anterior cruciate ligament reconstruction prevent development of meniscal damage? Results from a secondary analysis of a randomised controlled trial. Br J Sports Med. 2020;54(10):612-617. | X | ||
| Barfod KW, Hansen MS, Hölmich P, Kristensen MT, Troelsen A. Efficacy of early controlled motion of the ankle compared with immobilisation in non-operative treatment of patients with an acute Achilles tendon rupture: an assessor-blinded, randomised controlled trial. Br J Sports Med. 2020;54(12):719-724. | X | ||
| O’Keeffe M, O’Sullivan P, Purtill H, Bargary N, O’Sullivan K. Cognitive functional therapy compared with a group-based exercise and education intervention for chronic low back pain: a multicentre randomised controlled trial (Rct). Br J Sports Med. 2020;54(13):782-789. | X | ||
| Hinman RS, Campbell PK, Lawford BJ, et al. Does telephone-delivered exercise advice and support by physiotherapists improve pain and/or function in people with knee osteoarthritis? Telecare randomised controlled trial. Br J Sports Med. 2020;54(13):790-797. | X | ||
| Emery CA, van den Berg C, Richmond SA, et al. Implementing a junior high school-based programme to reduce sports injuries through neuromuscular training (Isprint): a cluster randomised controlled trial (Rct). Br J Sports Med. 2020;54(15):913-919. | X | ||
| Åkerlund I, Waldén M, Sonesson S, Hägglund M. Forty-five per cent lower acute injury incidence but no effect on overuse injury prevalence in youth floorball players (Aged 12-17 years) who used an injury prevention exercise programme: two-armed parallel-group cluster randomised controlled trial. Br J Sports Med. 2020;54(17):1028-1035. | X | ||
| Pas HIMFL, Pluim BM, Kilic O, et al. Effectiveness of an e-health tennis-specific injury prevention programme: randomised controlled trial in adult recreational tennis players. Br J Sports Med. 2020;54(17):1036-1041. | X | ||
| Matthews M, Rathleff MS, Claus A, et al. Does foot mobility affect the outcome in the management of patellofemoral pain with foot orthoses versus hip exercises? A randomised clinical trial. Br J Sports Med. 2020;54(23):1416-1422. | X | ||
| Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish degenerative meniscus lesion study) trial. Br J Sports Med. 2020;54(22):1332-1339. | X | ||
| Harøy J, Clarsen B, Wiger EG, et al. The Adductor Strengthening Programme prevents groin problems among male football players: a cluster-randomised controlled trial. Br J Sports Med. 2019;53(3):150-157. | X | ||
| Sandal LF, Thorlund JB, Moore AJ, Ulrich RS, Dieppe PA, Roos EM. Room for improvement: a randomised controlled trial with nested qualitative interviews on space, place and treatment delivery. Br J Sports Med. 2019;53(6):359-367. | X | ||
| Swart NM, van Oudenaarde K, Bierma-Zeinstra SM, et al. Does MRI add value in general practice for patients with traumatic knee complaints? A 1-year randomised controlled trial. Br J Sports Med. 2019;53(20):1285-1292. | X | ||
| Beaudouin F, Rössler R, Aus der Fünten K, et al. Effects of the “11+ Kids” injury prevention programme on severe injuries in children’s football: a secondary analysis of data from a multicentre cluster-randomised controlled trial. Br J Sports Med. 2019;53(22):1418-1423. | X | ||
| Gardner T, Refshauge K, McAuley J, Hübscher M, Goodall S, Smith L. Combined education and patient-led goal setting intervention reduced chronic low back pain disability and intensity at 12 months: a randomised controlled trial. Br J Sports Med. 2019;53(22):1424-1431. | X | ||
| Fokkema T, de Vos R-J, van Ochten JM, et al. Online multifactorial prevention programme has no effect on the number of running-related injuries: a randomised controlled trial. Br J Sports Med. 2019;53(23):1479-1485. | X | ||
| Bonanno DR, Murley GS, Munteanu SE, Landorf KB, Menz HB. Effectiveness of foot orthoses for the prevention of lower limb overuse injuries in naval recruits: a randomised controlled trial. Br J Sports Med. 2018;52(5):298-302. | X | ||
| Attwood MJ, Roberts SP, Trewartha G, England ME, Stokes KA. Efficacy of a movement control injury prevention programme in adult men’s community rugby union: a cluster randomised controlled trial. Br J Sports Med. 2018;52(6):368-374. | X | ||
| Garcia AN, Costa L da CM, Hancock MJ, et al. McKenzie Method of Mechanical Diagnosis and Therapy was slightly more effective than placebo for pain, but not for disability, in patients with chronic non-specific low back pain: a randomised placebo controlled trial with short and longer term follow-up. Br J Sports Med. 2018;52(9):594-600. | X | ||
| Esculier J-F, Bouyer LJ, Dubois B, et al. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain?A randomised clinical trial. Br J Sports Med. 2018;52(10):659-666. | X | ||
| Hespanhol LC, van Mechelen W, Verhagen E. Effectiveness of online tailored advice to prevent running-related injuries and promote preventive behaviour in Dutch trail runners: a pragmatic randomised controlled trial. Br J Sports Med. 2018;52(13):851-858. | X | ||
| Iordens GIT, Van Lieshout EMM, Schep NWL, et al. Early mobilisation versus plaster immobilisation of simple elbow dislocations: results of the FuncSiE multicentre randomised clinical trial. Br J Sports Med. 2017;51(6):531-538. | X | ||
| Iordens GIT, Van Lieshout EMM, Schep NWL, et al. Early mobilisation versus plaster immobilisation of simple elbow dislocations: results of the FuncSiE multicentre randomised clinical trial. Br J Sports Med. 2017;51(6):531-538. | X | ||
| Andersson SH, Bahr R, Clarsen B, Myklebust G. Preventing overuse shoulder injuries among throwing athletes: a cluster-randomised controlled trial in 660 elite handball players. Br J Sports Med. 2017;51(14):1073-1080. | X | ||
| Hislop MD, Stokes KA, Williams S, et al. Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial. Br J Sports Med. 2017;51(15):1140-1146. | X | ||
| Giles L, Webster KE, McClelland J, Cook JL. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. Br J Sports Med. 2017;51(23):1688-1694. | X | ||
| Schrøder CP, Skare Ø, Reikerås O, Mowinckel P, Brox JI. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. Br J Sports Med. 2017;51(24):1759-1766. | X | ||
| Ford JJ, Hahne AJ, Surkitt LD, et al. Individualised physiotherapy as an adjunct to guideline-based advice for low back disorders in primary care: a randomised controlled trial. Br J Sports Med. 2016;50(4):237-245. | X | ||
| Malisoux L, Chambon N, Delattre N, Gueguen N, Urhausen A, Theisen D. Injury risk in runners using standard or motion control shoes: a randomised controlled trial with participant and assessor blinding. Br J Sports Med. 2016;50(8):481-487. | X | ||
| Zebis MK, Andersen LL, Brandt M, et al. Effects of evidence-based prevention training on neuromuscular and biomechanical risk factors for ACL injury in adolescent female athletes: a randomised controlled trial. Br J Sports Med. 2016;50(9):552-557. | X | ||
| Kiadaliri AA, Englund M, Lohmander LS, Carlsson KS, Frobell RB. No economic benefit of early knee reconstruction over optional delayed reconstruction for ACL tears: registry enriched randomised controlled trial data. Br J Sports Med. 2016;50(9):558-563. | X | ||
| James AM, Williams CM, Haines TP. Effectiveness of footwear and foot orthoses for calcaneal apophysitis: a 12-month factorial randomised trial. Br J Sports Med. 2016;50(20):1268-1275. | X | ||
| Coombes BK, Connelly L, Bisset L, Vicenzino B. Economic evaluation favours physiotherapy but not corticosteroid injection as a first-line intervention for chronic lateral epicondylalgia: evidence from a randomised clinical trial. Br J Sports Med. 2016;50(22):1400-1405. | X | ||
| Wall PD, Dickenson EJ, Robinson D, et al. Personalised Hip Therapy: development of a non-operative protocol to treat femoroacetabular impingement syndrome in the FASHIoN randomised controlled trial. Br J Sports Med. 2016;50(19):1217-1223. | X | ||
| Hebert JJ, Fritz JM, Thackeray A, Koppenhaver SL, Teyhen D. Early multimodal rehabilitation following lumbar disc surgery: a randomised clinical trial comparing the effects of two exercise programmes on clinical outcome and lumbar multifidus muscle function. Br J Sports Med. 2015;49(2):100-106. | X | ||
| Chuter VH, de Jonge XAKJ, Thompson BM, Callister R. The efficacy of a supervised and a home-based core strengthening programme in adults with poor core stability: a three-arm randomised controlled trial. Br J Sports Med. 2015;49(6):395-399. | X | ||
| Rathleff MS, Roos EM, Olesen JL, Rasmussen S. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med. 2015;49(6):406-412. | X | ||
| Hamilton B, Tol JL, Almusa E, et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial. Br J Sports Med. 2015;49(14):943-950. | X | ||
| Munteanu SE, Scott LA, Bonanno DR, et al. Effectiveness of customised foot orthoses for Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2015;49(15):989-994. | X | ||
| Ng L, Cañeiro JP, Campbell A, Smith A, Burnett A, O’Sullivan P. Cognitive functional approach to manage low back pain in male adolescent rowers: a randomised controlled trial. Br J Sports Med. 2015;49(17):1125-1131. | X | ||
| Reurink G, Goudswaard GJ, Moen MH, et al. Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: the Dutch Hamstring Injection Therapy study. Br J Sports Med. 2015;49(18):1206-1212. | X | ||
| Rio E, Kidgell D, Purdam C, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49(19):1277-1283. | X | ||
| Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial. Br J Sports Med. 2014;48(4):332-338. | X | ||
| Askling CM, Tengvar M, Tarassova O, Thorstensson A. Acute hamstring injuries in Swedish elite sprinters and jumpers: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2014;48(7):532-539. | X | ||
| Janssen KW, van Mechelen W, Verhagen EALM. Bracing superior to neuromuscular training for the prevention of self-reported recurrent ankle sprains: a three-arm randomised controlled trial. Br J Sports Med. 2014;48(16):1235-1239. | X | ||
| Schneider KJ, Meeuwisse WH, Nettel-Aguirre A, et al. Cervicovestibular rehabilitation in sport-related concussion: a randomised controlled trial. Br J Sports Med. 2014;48(17):1294-1298. | X | ||
| Lindblom H, Waldén M, Carlfjord S, Hägglund M. Implementation of a neuromuscular training programme in female adolescent football: 3-year follow-up study after a randomised controlled trial. Br J Sports Med. 2014;48(19):1425-1430. | X | ||
| Hallgren HCB, Holmgren T, Oberg B, Johansson K, Adolfsson LE. A specific exercise strategy reduced the need for surgery in subacromial pain patients. Br J Sports Med. 2014;48(19):1431-1436. | X | ||
| Steunebrink M, Zwerver J, Brandsema R, Groenenboom P, van den Akker-Scheek I, Weir A. Topical glyceryl trinitrate treatment of chronic patellar tendinopathy: a randomised, double-blind, placebo-controlled clinical trial. Br J Sports Med. 2013;47(1):34-39. | X | ||
| Steffen K, Meeuwisse WH, Romiti M, et al. Evaluation of how different implementation strategies of an injury prevention programme (FIFA 11+) impact team adherence and injury risk in Canadian female youth football players: a cluster-randomised trial. Br J Sports Med. 2013;47(8):480-487. | X | ||
| Nauta J, Knol DL, Adriaensens L, Klein Wolt K, van Mechelen W, Verhagen EALM. Prevention of fall-related injuries in 7-year-old to 12-year-old children: a cluster randomised controlled trial. Br J Sports Med. 2013;47(14):909-913. | X | ||
| Askling CM, Tengvar M, Thorstensson A. Acute hamstring injuries in Swedish elite football: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2013;47(15):953-959. | X | ||
| Bredeweg SW, Zijlstra S, Bessem B, Buist I. The effectiveness of a preconditioning programme on preventing running-related injuries in novice runners: a randomised controlled trial. Br J Sports Med. 2012;46(12):865-870. | X | ||
| Andersen CH, Andersen LL, Gram B, et al. Influence of frequency and duration of strength training for effective management of neck and shoulder pain: a randomised controlled trial. Br J Sports Med. 2012;46(14):1004-1010. | X | ||
| van Beijsterveldt AMC, van de Port IGL, Krist MR, et al. Effectiveness of an injury prevention programme for adult male amateur soccer players: a cluster-randomised controlled trial. Br J Sports Med. 2012;46(16):1114-1118. | X | ||
| de Vos RJ, Weir A, Tol JL, Verhaar J a. N, Weinans H, van Schie HTM. No effects of PRP on ultrasonographic tendon structure and neovascularisation in chronic midportion Achilles tendinopathy. Br J Sports Med. 2011;45(5):387-392. | X | ||
| Alfredson H. Ultrasound and Doppler-guided mini-surgery to treat midportion Achilles tendinosis: results of a large material and a randomised study comparing two scraping techniques. Br J Sports Med. 2011;45(5):407-410. | X | ||
| Willberg L, Sunding K, Forssblad M, Fahlström M, Alfredson H. Sclerosing polidocanol injections or arthroscopic shaving to treat patellar tendinopathy/jumper’s knee? A randomised controlled study. Br J Sports Med. 2011;45(5):411-415. | X | ||
| Yelland MJ, Sweeting KR, Lyftogt JA, Ng SK, Scuffham PA, Evans KA. Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med. 2011;45(5):421-428. | X | ||
| Singer BJ, Silbert PL, Song S, Dunne JW, Singer KP. Treatment of refractory anterior knee pain using botulinum toxin type A (Dysport) injection to the distal vastus lateralis muscle: a randomised placebo controlled crossover trial. Br J Sports Med. 2011;45(8):640-645. | X | ||
| Hirschmüller A, Baur H, Müller S, Helwig P, Dickhuth H-H, Mayer F. Clinical effectiveness of customised sport shoe orthoses for overuse injuries in runners: a randomised controlled study. Br J Sports Med. 2011;45(12):959-965. | X | ||
| Creaney L, Wallace A, Curtis M, Connell D. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomised trial of autologous blood injections versus platelet-rich plasma injections. Br J Sports Med. 2011;45(12):966-971. | X | ||
| Hirschmüller A, Baur H, Müller S, Helwig P, Dickhuth H-H, Mayer F. Clinical effectiveness of customised sport shoe orthoses for overuse injuries in runners: a randomised controlled study. Br J Sports Med. 2011;45(12):959-965. | X | ||
| Emery CA, Meeuwisse WH. The effectiveness of a neuromuscular prevention strategy to reduce injuries in youth soccer: a cluster-randomised controlled trial. Br J Sports Med. 2010;44(8):555-562. | X | ||
| Giannetti BM, Staiger C, Bulitta M, Predel H-G. Efficacy and safety of comfrey root extract ointment in the treatment of acute upper or lower back pain: results of a double-blind, randomised, placebo controlled, multicentre trial. Br J Sports Med. 2010;44(9):637-641. | X | ||
| de Jonge S, de Vos RJ, Van Schie HTM, Verhaar J a. N, Weir A, Tol JL. One-year follow-up of a randomised controlled trial on added splinting to eccentric exercises in chronic midportion Achilles tendinopathy. Br J Sports Med. 2010;44(9):673-677. | X | ||
| Jamtvedt G, Herbert RD, Flottorp S, et al. A pragmatic randomised trial of stretching before and after physical activity to prevent injury and soreness. Br J Sports Med. 2010;44(14):1002-1009. | X | ||
| Paoloni JA, Murrell G a. C, Burch RM, Ang RY. Randomised, double-blind, placebo-controlled clinical trial of a new topical glyceryl trinitrate patch for chronic lateral epicondylosis. Br J Sports Med. 2009;43(4):299-302. | X | ||
| Zeisig E, Fahlström M, Ohberg L, Alfredson H. Pain relief after intratendinous injections in patients with tennis elbow: results of a randomised study. Br J Sports Med. 2008;42(4):267-271. | X | ||
| Sellwood KL, Brukner P, Williams D, Nicol A, Hinman R. Ice-water immersion and delayed-onset muscle soreness: a randomised controlled trial. Br J Sports Med. 2007;41(6):392-397. | X | ||
| de Vos RJ, Weir A, Visser RJA, de Winter T, Tol JL. The additional value of a night splint to eccentric exercises in chronic midportion Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2007;41(7):e5. | X | ||
| Bjordal JM, Lopes-Martins R a. B, Iversen VV. A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med. 2006;40(1):76-80. | X | ||
| Brown R, Orchard J, Kinchington M, Hooper A, Nalder G. Aprotinin in the management of Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2006;40(3):275-279. | X | ||
| Osborne HR, Allison GT. Treatment of plantar fasciitis by LowDye taping and iontophoresis: short term results of a double blinded, randomised, placebo controlled clinical trial of dexamethasone and acetic acid. Br J Sports Med. 2006;40(6):545-549. | X | ||
| Bleakley CM, McDonough SM, MacAuley DC, Bjordal J. Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. Br J Sports Med. 2006;40(8):700-705. | X | ||
| Huguenin L, Brukner PD, McCrory P, Smith P, Wajswelner H, Bennell K. Effect of dry needling of gluteal muscles on straight leg raise: a randomised, placebo controlled, double blind trial. Br J Sports Med. 2005;39(2):84-90. | X | ||
| Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39(2):91-96. | X | ||
| Young MA, Cook JL, Purdam CR, Kiss ZS, Alfredson H. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med. 2005;39(2):102-105. | X | ||
| Gunter P, Schwellnus MP. Local corticosteroid injection in iliotibial band friction syndrome in runners: a randomised controlled trial. Br J Sports Med. 2004;38(3):269-272. | X | ||
| Predel HG, Koll R, Pabst H, et al. Diclofenac patch for topical treatment of acute impact injuries: a randomised, double blind, placebo controlled, multicentre study. Br J Sports Med. 2004;38(3):318-323. | X | ||
| Haake M, Buch M, Schoellner C, et al. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ. 2003;327(7406):75. | X | ||
| Kerkhoffs GMMJ, Struijs P a. A, de Wit C, Rahlfs VW, Zwipp H, van Dijk CN. A double blind, randomised, parallel group study on the efficacy and safety of treating acute lateral ankle sprain with oral hydrolytic enzymes. Br J Sports Med. 2004;38(4):431-435. | X | ||
| Wetzel D, Menke W, Dieter R, Smasal V, Giannetti B, Bulitta M. Escin/diethylammonium salicylate/heparin combination gels for the topical treatment of acute impact injuries: a randomised, double blind, placebo controlled, multicentre study. Br J Sports Med. 2002;36(3):183-188. | X |




[…] – Udgivet 4. februar 2022 0 […]