Ultrasound guided needling vs. extracorporeal shockwave for the treatment of calcific tendinitis in the rotator cuff
“Bite sized Science” by Jonathan Vela, MD
Dept. of Rheumatology Aalborg Denmark
Email: j.vela@rn.dk
Calcific tendinitis and associated inflammation of the rotator cuff is a frequently occurring disorder in which anti-inflammatory medication, exercise therapy and corticosteroid injection are recommended as first line treatments. More invasive techniques like shock wave and ultrasound guided needling (UGN see BOX1) can be utilized prior to arthroscopy. But is UGN or shockwave preferable? Louwerens et al. examined this in a randomized controlled study from February 2020.
Participants had subacromial pain syndrome and a concurrent calcification in a rotator cuff tendon with a diameter of ³ 5 mm. Participation required shoulder pain ³ four months and insufficient relief from physiotherapy, anti-inflammatory medication and a subacromial corticosteroid injection. Participants with partial or full rotator cuff rupture were excluded.
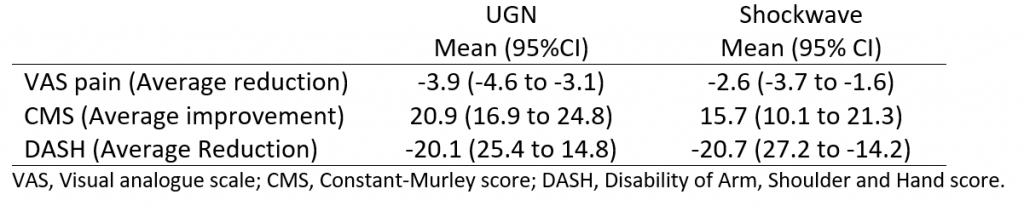
Randomization was done electronically but blinding of participants was not possible due to the nature of the treatments. A total of 82 patients participated in the study. On average, they were 52 years old, had been symptomatic for ³ three years and their pain intensity were equivalent to 5.9 cm on a 10 cm visual analogue scale (VAS). Clinical outcomes were measured after one year and included pain intensity (VAS), function (Constant-Murley Score) and disability (Disability of Arm, Shoulder and Hand score) (see table 1 for relative effect)
Table 1. Relative effect of treatment after one year.
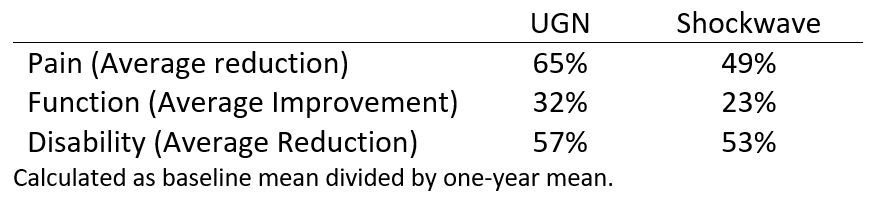
Figure 1.

Table 2. Effect of treatment after one year.
BOX 1. Ultrasound guided needling
Ultrasound guided needling, also known as barbotage, is an ultrasound guided lavage technique using two needles. The calcification is punctured multiple times with one needle while aspiration and lavage is performed with the other. The procedure is done using local anaesthetic and corticosteroid injection to minimize inflammation.
None of the treatments had serious side effects but patients reported experiencing greater pain during shockwave treatment versus UGN (6.2 cm vs. 4.5 cm on a 10 cm VAS). In addition, 41% of patients receiving shockwave had additional treatment versus 22% in the UGN group. In the shockwave group, additional treatment consisted of arthroscopy with removal of bursa (7 patients), conversion to UGN (5 patients) and corticosteroid injection (5 patients). In the UGN group, the additional treatment consisted of corticosteroid injection (9 patients).
The study was well performed. The authors addressed several limitations in the discussion including the lack of a control group receiving no treatment. Here the authors explained that they tried to compensate for a lack of a “waiting list group” by only including patients who had failed previous conservative treatment.
Both treatments were effective, but UGN led to better results in pain reduction, increased function and decreased disability scores. Furthermore, UGN as a treatment was less painful and patients receiving UGN required fewer additional invasive treatments. It should be noted that the results presented are for the intention to treat analysis, thus the effect of shockwave alone could be less then reported.
For patients with subacromial pain syndrome due to calcific tendinitis and insufficient relief from physiotherapy, anti-inflammatory medication and a subacromial corticosteroid injection – UGN would be the preferred treatment option and a skill that clinicians should master.
Reference:
Louwerens JKG, Sierevelt IN, Kramer ET, et al. Comparing ultrasound-guided needling combined with a subacromial corticosteroid injection versus high-energy extracorporeal shockwave therapy for calcific tendinitis of the rotator cuff. A randomized controlled trial. Arthrosc J Arthrosc Relat Surg. 2020:1-11. doi:10.1016/j.arthro.2020.02.027