Femoroacetabular impingement syndrome: Treatment and clinical decision making
Erik Poulsen, postdoc
epoulsen@health.sdu.dk
Department of Sports Science and Clinical Biomechanics
University of Southern Denmark
Twitter: @UsefulHipStuff
In the last decade there has been an increased focus on activity-related hip and/or groin pain in younger individuals participating in sports, commonly diagnosed as femoroacetabular impingement (FAI) syndrome (1, 2). Following clinical examination and imaging to confirm or rule out the diagnosis, a decision must be made regarding treatment followed by involving and engaging the patient in a decision-making process prior to consenting to treatment.
Healthcare and informed consent
By law, it is required to obtain informed consent prior to initiating any examination and treatment (3). This ‘informed’ consent involves informing the patient about the current evidence for different treatment options for the specific condition. It further includes information about potential harms of the proposed treatments (3). This enables the patient to participate actively in the decision-making process about the treatment.
Evidence-based practice
In addition to including current scientific evidence, the patient’s preference, concerns and expectation as well as the experience/’expertise’ of the clinician should be incorporated into the decision process (4).
Current evidence for treatment of FAI syndrome
What is the current evidence level for treatment of patients with FAI syndrome? So far, no systematic review and meta-analysis has been published comparing the two most commonly used treatment options: arthroscopic hip surgery and exercise therapy. However, within the last year, two large multicenter randomized clinical trials (RCT) have been published comparing hip arthroscopic surgery to either a personalized hip therapy program or an individual goal oriented exercise program including activity modification (5, 6).
To assist the clinician (as well as the patient) in the information and decision process, the following figures and table provide very short summaries of the results of these two recently published RCTs. The figures compare the primary outcome examined in the two trials and the table lists the benefits and harms between hip arthroscopic surgery and the non-surgical approach.
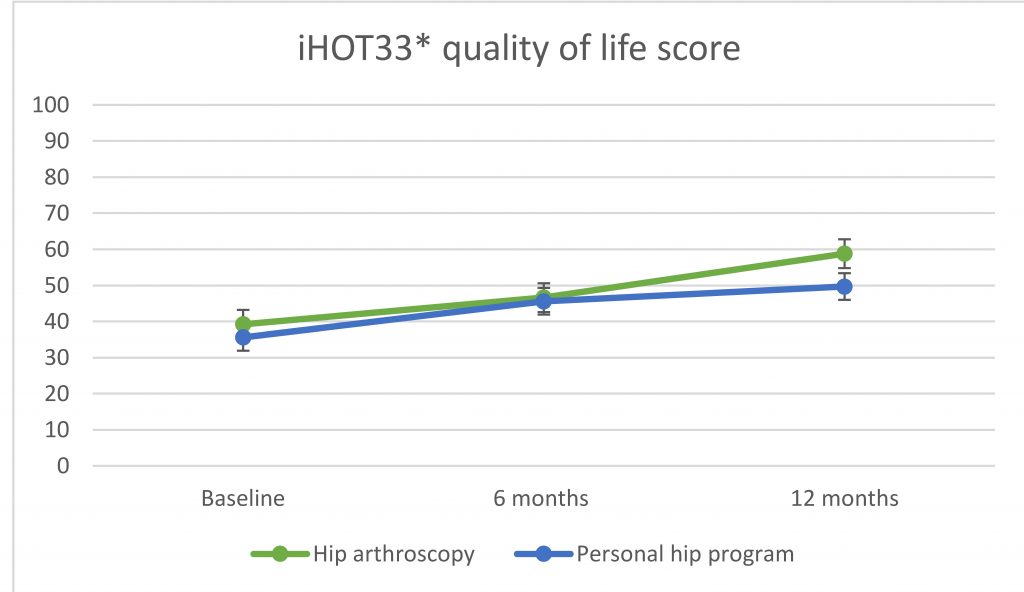
Figure 1. Primary outcome from Griffin et al. 2018 * international Hip Outcome Tool (0 = worst, 100 = best)
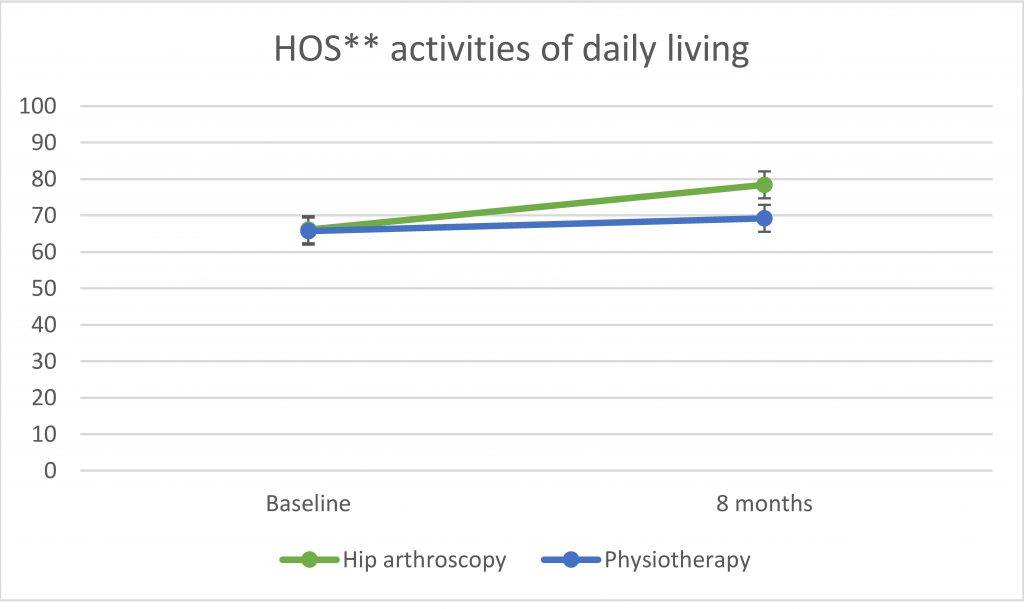
Figure 2. Primary outcome from Palmer et al. 2019 ** Hip Outcome Score (0 = worst, 100 = best)
Table 1. Change in patient-reported outcomes from baseline to final follow-up:
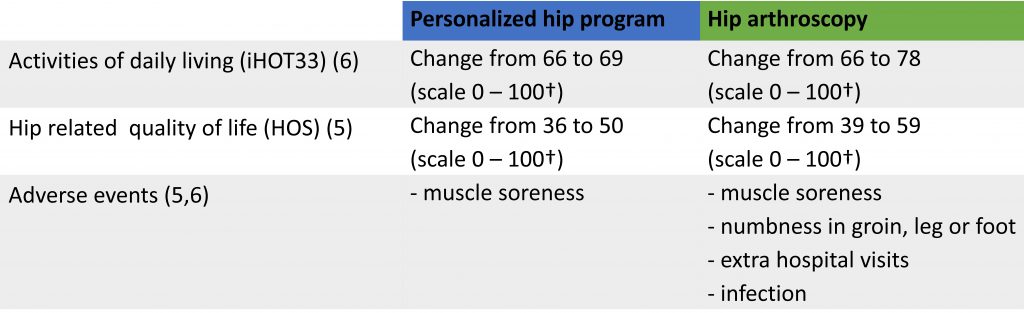
† (0 = worst, 100 = best)
In both studies, on average patients benefit significantly (but slightly) more from having hip arthroscopy in comparison to a personal exercise therapy program. However, neither groups are symptom free at any of the follow-ups and in the second study (6) the authors state: “Up to half of patients may not improve to a satisfactory clinical level after arthroscopic surgery” (6). This pertains as well for the non-surgical approach and information relevant to convey to the patient setting up treatment goals.
Additional information to the patient prior to decision-making
A large proportion of individuals diagnosed with FAI syndrome have participated or still participate in sports at various levels. However, not all are able to return to the same level of their sport following .e.g. hip arthroscopic surgery. Recent studies report different rates of returning to sports at pre-injury level ranging between 57-82% (7-9). This indicates expectations levels from any of the treatment methods should be modified accordingly. In addition, no strong evidence is available about predictors informing which patients with FAI syndrome will benefit the most from hip arthroscopic surgery or a non-surgical treatment regime. Further, proposing that surgery for cam, pincer and/or labral tears will prevent or delay development of osteoarthritis in the hip is speculative. No sufficient evidence with the relevant long-term follow-up is currently available to support this. Lastly, hip arthroscopic surgery for cam, pincer and labral tears in the middle age and older (>40 years) have less favorable results compared to surgery in the younger population (10).
Conclusion – empowering the patient
Informing and applying the current evidence including benefits and harms of possible treatment options in a format comprehensible to the patient will allow for an informed decision based on individual preferences and concerns. This process will require time, both for the clinician and for patient comprehension. However, the time is well spend and essential for the future wellbeing of the patient and will likely improve compliance with treatment.
References
- Kemp J, Grimaldi A, Heerey J, Jones D, Scholes M, Lawrenson P, et al. Current trends in sport and exercise hip conditions: Intra-articular and extra-articular hip pain, with detailed focus on femoroacetabular impingement (FAI) syndrome. Best practice & research Clinical rheumatology. 2019;33(1):66-87.
- Thorborg K, Rathleff MS, Petersen P, Branci S, Holmich P. Prevalence and severity of hip and groin pain in sub-elite male football: a cross-sectional cohort study of 695 players. Scandinavian journal of medicine & science in sports. 2017;27(1):107-14.
- Sundhedsloven – Afsnit III: Patienters retsstilling – kapitel 5: Patienters medinddragelse i beslutninger §15 og §16, (2018).
- Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine, how to practice and teach EBM. 2nd ed. London: Churchill Livingstone; 2000.
- Griffin DR, Dickenson EJ, Wall PDH, Achana F, Donovan JL, Griffin J, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225-35.
- Palmer AJR, Ayyar Gupta V, Fernquest S, Rombach I, Dutton SJ, Mansour R, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. Bmj. 2019;364:l185.
- Reiman MP, Peters S, Sylvain J, Hagymasi S, Mather RC, Goode AP. Femoroacetabular impingement surgery allows 74% of athletes to return to the same competitive level of sports participation but their level of performance remains unreported: a systematic review with meta-analysis. British journal of sports medicine. 2018.
- Memon M, Kay J, Hache P, Simunovic N, Harris JD, O’Donnell J, et al. Athletes experience a high rate of return to sport following hip arthroscopy. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2018.
- Ishoi L, Thorborg K, Kraemer O, Holmich P. Return to Sport and Performance After Hip Arthroscopy for Femoroacetabular Impingement in 18- to 30-Year-Old Athletes: A Cross-sectional Cohort Study of 189 Athletes. The American journal of sports medicine. 2018:363546518789070.
- Horner NS, Ekhtiari S, Simunovic N, Safran MR, Philippon MJ, Ayeni OR. Hip Arthroscopy in Patients Age 40 or Older: A Systematic Review. Arthroscopy. 2017;33(2):464-75.e3.
Keywords: femoroacetabular impingement, treatment, hip arthroscopy, physiotherapy, clinical decision making, patient involvement, evidence-based practice.